A 45 year old female with viral pneumonia secondary to Covid-19
Roll .no : 36
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis “ to develop my competency in reading and comprehending clinical data including history,clinical findings,investigations, and come up with diagnosis and treatment plan.
A 45 year old female patient came to opd with Chief complaints of fever since 1week ,dry cough since 1week ,decreased appetite and chest pain during cough since 2 days.
History of presenting illness:
Patient was apparently asymptomatic 1 week back and she developed
fever which is insidious in onset ,relieved by medication and not associated with chills and rigors.
Dry cough since one week .
Chest pain since two days ,which is stabbing type of pain And aggravating during cough.
Past history:
She is not a known case of DM,HTN
Family history:
No significant family history
None of her family members are tested covid positive
Personal history:
Diet : vegetarian
Appetite: decreased
Sleep : adequate
Bowel and bladder movements:normal
No addictions
General examination:
The patient is conscious,coherent and cooperative and well oriented to time place and person . She is sitting comfortably on the bed,moderately built and well nourished .
Pallor: absent
Icterus:absent
Cyanosis: absent
Clubbing: absent
Lymphadenopathy: absent
Edema: absent
VITALS:
Temperature:afebrile
Pulse rate:90 bpm
Respiratory rate:24 /min
Blood pressure:110/70 mm Hg
SpO2 : 8O -85with room air
95% with 15 lit of O2
GRBS :200 mg/dL
SYSTEMIC EXAMINATION:
• Respiratory system: Normal vesicular breath sounds heard
• CVS: S1 and S2 heard
No added murmurs
•PA: soft and non tender ,
No organomegaly
•Central Nervous System: intact
INVESTIGATIONS:
•CBP:
Hb:12.9 gm%
TLC:4000 cells/mm3
DLC : neutrophils:67
Lymphocytes:28
Eosinophils:02
Monocytes:03
•CRP: positive
0.6 mg/dL
•D-Dimer: 1150 ng/ml
•serum LDH: 518 IU/lit
•LFT:
•ECG:
•Rapid antigen test: positive
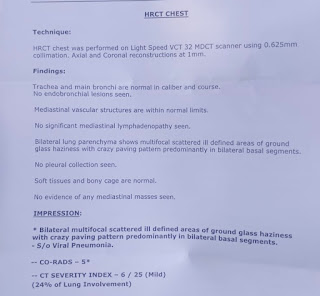
•HRCT :
•CORADS: 5
•CT SS : 6/25
Provisional diagnosis: Viral pneumonia secondary to covid-19 infection ,CTSS :6/25 and CORADS: 5
And denovo DM
Treatment:
O2 inhalation
Duolin budecort nebulization
Inj.Pantop OD
Inj.Clexane 40 mg BD
Inj.Dexamethasone 8mg OD
Tab.Mvt OD
Tab.Limcee OD
Tab.dolo sos
Inj.HAI 4 units TID
Syp.Grelinctus 10 mL TID
Update :
45year female
viral pnemonia secondary to COVID-19, denovo DM
Vitals
Bp : 110/70 mm hg
Pr 90 bpm RR- 22/min
Spo2 : 93with room air ,
95 with 5lit of O2
treatment
Prone positioning
02 inhalation
Duolin budecort nebulization
Inj Pantop od
Inj. Clexane 40mg BD
Inj. DEXAMETHASONE 8mg od
Tab. Mvt od
Tab. Limcee od
Tab.dolo sos
Inj. HAI 4units TID
Syp. Grillinctus 10ml tid
New onset of DM in Covid-19:
- Similar to SARS-CoV which caused an epidemic in 2002- 03, the novel coronavirus enters cell hosts through Angiotensin II Converting Enzyme receptor (ACE2). This receptor is found throughout the body and its pulmonary distribution explains, not only the respiratory clinical features, but also the acute respiratory distress syndrome that leads to severity of the disease.
- ACE2 receptor is found in the pancreas, both on exocrine cells and in the endocrine cells, that constitute pancreatic islets. Interestingly, its expression is also relevant in the endothelial cells of the microvasculature supplying beta-cells that produce insulin.
- As it has been postulated, upon the 2003-SARS pandemic, coronavirus spike protein enters the cells using the ACE2 receptor, initiating an inflammatory response that leads to apoptosis. Previous studies attempting to understand the pathophysiology of the SARS-CoV-2 infection over different organs and systems, have su- ggested that, following viral entrance and cell infection, ACE2 receptor is downregulated in lung tissue, which subsequently may trigger an inflammatory response.
- Although SARS-CoV-2 could directly impair insulin production of beta-cells, diminishing its function and disturb glucose metabolism, would that be enough to com- promise insulin production in a long-term manner and induce type 1 diabetes? Is there any immune mediated process? Or is ACE2 downregulation the factor at stake?
- One hypothesis could be that the cytokine storm - caused by the severe inflammatory response taking place in the lungs also targets the pancreas possibly causing diabetes .
- Other hypothesis is related to the role of the renin-angiotensin system (RAS) and its counterbalancing arm, the ACE2-Ang(1-7)-Mas axis on the development of diabetes. It has been shown previously how ACE2 decreased activity is detrimental for the development of acute respiratory distress syndrome (ARDS), verified both during the SARS-CoV epidemic as well during the current pandemic of COVID-19.
In recent years, it has also been proposed that stimulation of the ACE2-Ang(1-7)-Mas axis could be protective against deleterious effects of diabetic nephropathy, hypertension and diabetic retinopathy and that patients with diabetes have lower Angiotensin-(1-7) levels and lower activity of ACE2. These findings are consistent with the clinical features of patients infected by SARS- -CoV-2: that develop de novo hyperglycemia with difficult metabolic control, since there is downregulation of the ACE2 receptor which is internalized.
New onset DM in patient may be responsible for late recovery as the virus may thrive in an environment of elevated blood glucose.




Comments
Post a Comment