INTERN ASSESSMENT
G.Sai Vidya ,Roll .no:44
Forever grateful to the entire general medicine team for guiding me throughout my internship in GM department .
Thanks to Dr.Rakesh Biswas Sir (HOD)
Dr.Aditya Samitinjay Sir(SR)
And my unit PGs :Dr.Sai Charan Sir (PGY3),Dr.Shashikala Ma’am (PGY3),Dr.Deepika(PGY1),Dr.Kranthi (PGY1)
And thanks to all PGs and my cointerns :)
To be very honest ,I never thought I’d love medicine until my internship in medicine department ..every day there is a new thing to learn and new thing to discover ..it’s very fascinating yet simple if we have good hold of the concept ....
Connecting all the dots ,starting from history ,examination to sending labs to know what’s going wrong ...checking all the biochemical parameters ,microbiological and pathological parameters too
And reaching an ultimate anatomical or physiological localization of patient’s problem ..but sometimes some diagnosis remains a query(?)[because human body is full of wonders and somethings remain unanswered ]
In my one month of unit duty (12/10/22 to 11/11/22)
I had the best opportunity of working under Dr.Aditya Sir ,
in these 30 days I learnt :
-Updating fever and investigation charts daily and updating SOAP notes
-Plotting the trends of lab values graphically ,which helped me in deciding the prognosis of the disease
-Rounds are my favourite part ...where we discussed every patient in detail , initially discussing about the problem statement and then examination ..reaching a clinical diagnosis and later we discuss the patient’s lab results ,we refer to articles and research projects that helps us to reach the diagnosis,finally we reach the diagnosis (anatomical /physiological localisation of the problem )and then planned the management accordingly .
-Dr.Raveen sir (pgy3) explained in detail about the importance of SOAP notes and how to follow up accordingly ,evaluating every patient considering the subjective complaints ,objective observations and planning the management accordingly.daily follow up is the key ..!
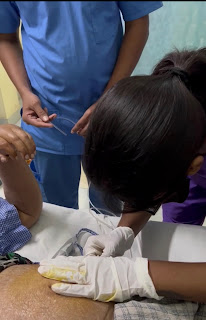
-got to do an ASCITIC TAP (therapeutic): Under the guidance of Dr.Venkat Sir (PGY1)
Video -
-Learnt how to shift an intubated case to dialysis
-learnt how to draw blood samples (venous and arterial samples )for routine lab investigations.
-Transfused blood for the following cases:
https://08arshewarpavankumar.blogspot.com/2022/09/20-yr-female-with-bl-pedal-edema.html
https://muralikrishna98.blogspot.com/2022/10/18-years-old-patient-came-to-opd-with.html
https://vidya36.blogspot.com/2022/11/a-70-f-with-background-of-endometrial.html
Sending the sample for crossmatching
Taking the consent for the transfusion
To start transfusion after checking the vitals
Monitoring pt during transfusion, keeping an eye on in case of any reactions during transfusion ,post transfusion vitals
-Assisted in extubation of a 80M https://sahithireddy158.blogspot.com/2022/10/80-year-old-male.html
-Camp day :visited an oldage home ,took history and monitored vitals of patients , And given treatment .
They were mostly diabetic and hypertensive
-A very interesting case of 40M with giddiness ,loose stools and yellowish discolouration of skin following ingestion of a Ayurvedic medicine
Link to the case : https://sahithireddy158.blogspot.com/2022/10/40-year-old-with-giddiness.html?m=1
Discussion around this case :
What was the name of the herbal medicine he took ?
Ravaseela gandha
https://pmj.bmj.com/content/79/933/391
"Arsenic continues to be an essential constituent of many non-western traditional medicine products. Some Chinese traditional medications contain realgar (arsenic sulphide) and are available as pills, tablets, and other preparations. They are used for psoriasis, syphilis, asthma, rheumatism, haemorrhoids, cough and pruritus, and are also prescribed as a health tonic, an analgesic, anti-inflammatory agent, and as a treatment for some malignant tumours.21–23 In India, herbal medicines containing arsenic are used in some homoeopathic preparations24 and haematological malignancies.25 In Korea arsenic is prescribed in herbal medicine for haemorrhoids.26"
Same applies to Lead, Thallium, Mercury, Cadmium and all those heavy metal toxicities
"Most cases of acute arsenic poisoning occur from accidental ingestion of insecticides or pesticides and less commonly from attempted suicide. Small amounts (<5 mg) result in vomiting and diarrhoea but resolve in 12 hours and treatment is reported not to be necessary.44"
"The clinical features initially invariably relate to the gastrointestinal system and are nausea, vomiting, colicky abdominal pain, and profuse watery diarrhoea. The abdominal pain may be severe and mimic an acute abdomen.49 Excessive salivation occurs50 and may be the presenting complaint in the absence of other gastrointestinal symptoms.51 Other clinical features are acute psychosis, a diffuse skin rash, toxic cardiomyopathy,47,52 and seizures.50"
"Diarrhoea attributed to increased permeability of the blood vessels is a dominant feature. The voluminous watery stools are described as “choleroid diarrhoea”. In cholera the stools are described as “rice water”, but in acute arsenic poisoning, because of blood in the gastrointestinal tract, the term “bloody rice water” diarrhoea is used. The cause of death is massive fluid loss due to secretion from the gastrointestinal tract eventuating in severe dehydration, reduced circulating blood volume, and consequent circulatory collapse. On postmortem examination oesophagitis, gastritis, and hepatic steatosis are reported.47"
"Haematological abnormalities reported are haemaglobinuria, intravascular coagulation, bone marrow depression, severe pancytopenia, and normocytic normochromic anaemia and basophilic stippling.52–54"
A case of 18 year old with anemia :
http://muralikrishna98.blogspot.com/2022/10/18-years-old-patient-came-to-opd-with.html
Discussion around this patient
Central pallor, microcytic hypochromic cells with tear drop cells and pencil forms
Cant find any macrocytes
A 17 year old female which background of hypothyroidism (a very young onset) with excellent clinical findings
https://abhirambhashyakarla.blogspot.com/2022/11/17-year-old-female-with-vomitings-and.html?m=1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6506997/
"The diagnosis of autoimmune Addison disease at autopsy is aided by several factors including 1) history, including salt craving, features consistent with orthostatic hypotension, and GI complaints including nausea, vomiting and pain, 2) physical examination findings of increased pigmentation and small or unidentifiable adrenal glands, 3) serologic testing for 21-hydroxylase antibodies, 4) serum cortisol concentrations, and 5) vitreous electrolyte testing. "
"The most specific symptoms of Addison disease are increased skin or oral mucosa pigmentation, hypotension, and salt craving (13). Increased pigmentation is most frequently found in the palmar creases, the buccal mucosa, and the extensor surfaces of the body, but can occur anywhere (1, 4, 14, 17)."
"The clinical diagnosis of Addison disease is made by checking a morning basal cortisol concentration, often around 0800 hrs (1, 2). A result of <3 μg/dL indicates adrenal insufficiency (2, 4, 14); however, some advocate a cut-off of <5 μg/dL (1). A concentration of 18 μg/dL or higher excludes adrenal insufficiency. If the result of a morning cortisol concentration testing is equivocal (i.e., 3.1 to 17.9 μg/L), a stimulation test can be performed”
Autoimmune destruction of the adrenal glands, also known as autoimmune adrenalitis, is now the most common cause of Addison disease in both children and adults.
Hyperpigmentation of the skin and mucosal surfaces, the most specific sign of Addison disease, occurs in up to 92% of patients. This dyspigmentation may precede other manifestations by up to 10 years.
We did an ACTH stimulation test to rule out/rule in Addisons ...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3262370/
"Administration is by intravenous or intramuscular injection and a rise in cortisol should generally be seen around 30 minutes after administration. Plasma cortisol levels usually peak about 45 to 60 minutes after injection and a normal response is an approximate doubling of the basal plasma cortisol value. A number of other agents may interfere with cosyntropin function and subsequent response. These include metyrapone, etomidate, ketoconazole, megesterol, and mitotate to name a few. In addition, agents such as rifampin and phenytoin may increase cortisol metabolism."
"Side effects of cosyntropin include nausea, anxiety, sweating, dizziness, itchy skin, redness and or swelling at injection site, palpitations, and facial flushing.18 Rarely seen side effects include fainting, headache, blurred vision, severe swelling, severe dizziness, trouble breathing, or an irregular heartbeat"
Inj Avil was given before the test
https://onlinelibrary.wiley.com/doi/10.1002/ajh.25749
Pica (allotriophagia), the compulsive craving and consumption of non-food substances, is a well-documented symptom associated with iron deficiency anemia (IDA). Commonly consumed substances include ice (pagophagia), cornstarch (amylophagia), and clay (geophagia).
The most widely accepted micronutrient deficiency hypothesis holds that patients consume non-food items in an attempt to augment deficiencies of iron, zinc, or other micronutrients. However, this hypothesis cannot explain pagophagia, as ice typically contains few trace minerals or iron. Other theories hold that ice consumption may counter reductions in alertness and central processing speed via changes in cerebral blood flow (dive reflex or sympathetic nervous system activation) or that ice consumption4 reflects an effort to soothe the glossitis that can accompany some micronutrient deficiencies.
Patient and attendees have been explained about Addisonian crisis and the warning signs and a PaJr group was created and discharged .
A 52 YEAR OLD MALE ,PRESENTED WITH CHIEF COMPLAINT OF PAIN ABDOMEN SINCE 20 YEARS
Decreased bowel movements (constipation) since 20 years
https://vidya36.blogspot.com/2022/10/a-52-year-old-male-with-background-of.html
Chronic mesenteric ischemia and CAD
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6929593/
Upper GI endoscopy: https://youtu.be/wisd9K1__3E
https://teachmesurgery.com/vascular/peripheral/chronic-mesenteric-ischaemia/
The gradual build-up of atherosclerotic plaque within the mesenteric vessels narrows the lumen, impairing blood flow to the supplied viscera, resulting in an inadequate blood supply to the bowel.
The classical set of symptoms associated with chronic mesenteric ischaemia are:
- Postprandial pain – classically occurring around 10mins-4hrs after eating*
- Weight loss – a combination of decreased calorie intake and malabsorption
- Concurrent vascular co-morbidities, e.g. previous MI, stroke, or PVD
Other less specific symptoms may include change in bowel habit (typically loose), nausea, and vomiting. Examination findings are often non specific; evidence of malnutrition/cachexia, generalised abdominal tenderness, and abdominal bruits may be present.
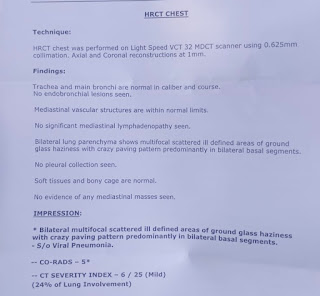
A 60 year old chronic smoker with COPD:
https://vidya36.blogspot.com/2022/10/60-years-old-male-with-sob.html
Anti cholinergics
The pooled results of 9 randomized placebo-controlled trials (Table 1) that ranged from three months to five years in duration (Salpeter, Buckley, Salpeter 2006) showed that anticholinergics reduced the risk of COPD hospitalizations by 30% and reduced respiratory deaths by 70%, compared with placebo (Figure 1). No significant effect on total mortality was seen.
Beta agonist
The pooled results of 9 randomized-placebo controlled trials (Table 1) lasting from three to 12 months (Salpeter and Buckley 2006; Salpeter, Buckley, Salpeter 2006) showed that β-agonist use increased respiratory deaths by over twofold compared with placebo, without significantly affecting hospitalizations or total mortality (Figure 2).
Seven trials directly compared β-agonists with anticholinergics in COPD (Table 1) and reported on hospitalizations or deaths (Salpeter and Buckley 2006; Salpeter, Buckley, Salpeter 2006). β-agonist use was associated with a two-fold increased risk for hospitalizations and a five-fold increased risk for total mortality compared with anticholinergic use (Figure 3). Four additional trials evaluated the combination of anticholinergics and β-agonists (Table 1); pooled results found that the combination was not better than anticholinergic use alone on these long-term clinical outcomes.
AR signs :
A 33F with hypothyroidism:
https://vidya36.blogspot.com/2022/10/a-33-year-old-female-with-background-of.html
Oral submucous fibrosis can be seen at any age except for young children. The predominant age group affected is 20-40 years. Compared to traditional betel quid, gutkha chewing tends to begin at a younger age and has a shorter time to the development of disease, so cases of oral submucous fibrosis have been seen as young as 11 years of age.
In some populations there was a female predominance, suggesting a possible hormonal influence or role for iron deficiency. More recently, with the ready availability of prepackaged commercial forms, a male predominance is now being reported.
The duration of betel quid chewing before the development of oral submucous fibrosis varies from a few months to many years, probably dependent on the composition of the quid and extent of the habit as well as genetic and other susceptibility factors.
Predisposing susceptibility factors such as genetic background may influence the development of oral submucous fibrosis with areca nut exposure. Rare families have been reported with this condition, yet have no betel quid chewing habit. An increased incidence of some specific tissue types have been identified.
https://dermnetnz.org/topics/oral-submucous-fibrosis
A 70 F with background of cervical cancer with foreground of anemia
https://vidya36.blogspot.com/2022/11/a-70-f-with-background-of-endometrial.html
Apical impulse visible and appeared to be heaving. Apex beat more than 10cm from midsternal line, in 6th ICS, larger than a 2 rupee coin and heaving. No palpable heart sounds.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5797745/
Reactive oxygen species formation has been shown to be an important factor in the development of RICVD, and decreased ability to clear free radicals causes a worsening of cardiovascular effects (19). ROS formation in healthy endothelial cells and subsequent signaling via NF-κB leads to an inflammatory state via expression of interleukin-1, interleukin-6, tumor necrosis factor-α (40), intercellular adhesion molecule-1 (41), and matrix metalloproteinases (42, 43). ROS levels remain elevated long after exposure to radiation. In animal models whose hearts were directly exposed to high-LET radiation, inflammation and apoptosis were shown to persist for at least 6 months (43, 44). This prolonged inflammation leads to a persistent but ineffective healing and remodeling response (45) marked by chronic inflammation of macrophages and mononuclear cells (46). The chronic inflammatory response is necessary for remodeling of damaged tissues, but the low levels of inflammation seen early in RICVD may be ineffective to fully restore tissue structure and function (47). Further, angiogenesis is disturbed after exposure to radiation due to the decrease in vascular endothelial growth factor secretion (48) and decreased tubule formation (14). The continuous attempts at repair induce the physiologic formation of more ROS (47), which contributes to a smoldering continuous inflammatory state. The vasculature’s inability to appropriately remodel from the initial radiation injury is further worsened by a decrease of endothelium-dependent relaxation (49, 50) worsening the effect of turbulent blood flood, another important factor in atherosclerotic development (51). Later, intimal thickening and atherosclerosis occurs, especially at areas of disturbed flow
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3487569/#!po=1.35135
"Close to 90% of patients will have profound fatigue, weight loss, and edema. Edema may have multiple causes, including hypoalbuminemia (from kidney, bowel, or liver involvement), right-heart failure, or simply the impairment of the blood vessels’ ability to handle hydrostatic pressure challenges. Other presenting symptoms depend on the organs most prominently involved in a given patient. Liver involvement is seen in 15-25% of patients, neuropathy in 15-20%, and cardiac involvement in up to 50%.9 Symptomatic heart failure, seen in 25-33% of patients, portends a median survival of less than 6 months.10 Renal involvement manifests as nephrotic syndrome. Involvement of the gastrointestinal tract causes macroglossia, diarrhea due to malabsorption, gastric hypomotility, and constipation. In 30% of patients, three or more organs are involved.7"
Abdominal fat pad aspiration was done:
Link to the video :
Fat pad aspiration is a relatively low cost and noninvasive method for obtaining tissue to diagnose systemic amyloidosis. This article describes fat pad aspiration procedure along with details about sample processing to submit specimen for both Congo red staining and ultrastructural evaluation by electron microscopy. In this video, we demonstrate this reproducible and simple procedure to retrieve optimal diagnostic material.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185617/
-A 60M HbsAg + with gross ascites and astrexis :
During Nephro duty :(under Dr.Sai Charan sir ,Dr.Keerthi mam )
-Collected blood samples for routine investigations
-Monitoring all the patients ,daily follow up with reports
-Monitored patients before during and after dialysis
-Inserted Foleys catheter
-Removal of foleys
- Renal Biopsy in a 30F :
-Hemoglobin levels in dialysis patients
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3431367/
During ward duty :(under Dr.Haripriya mam ,Dr.Shailesh sir )
SOAP notes update
Regular follow up of Ward patients
Helped my juniors in taking history and examination
taught (3rd sem students) the respiratory system examination
Attended classes (by Dr.Haripriya mam ,Dr.Vamshi sir) :few learning points -
-What medication to be given in case of hypertension pts depending on one’s age
-PRONE Ventilation and it’s significance
-how to differentiate between fine and coarse crepts (a beautiful example of paper and cardboard movements respectively)
During ICU duty :(under Dr.Vinay sir ,Dr.Deepika mam)
-Monitoring patients in ICU and AMC
-Setting up of IV drip ,Infusion ,Nebulisation
-Drawing samples
-IV cannula (for two patients )
-CPR for a 47M (thanks to Dr.Durga krishna sir and Dr.Deepika mam)
https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/algorithms
-Learnt how to use a defibrillator
-Learnt how to communicate with patients and their families and how to enclose about patients condition to their attendees
-Nursing stafff taught me how to set up an infusion drip
-Felt a diffuse apex beat in a 75F with Atrial Fibrillation and heart failure
-another interesting case of 30 F with loss of appetite,SOB ..learnt the technique of auscultation for pulmonary fibrosis .
-Assisted in emergency intubation (under Dr.Sai charan sir and Dr.Deepika mam )
-A case of Multi organ dysfunction syndrome secondary to E.Coli urosepsis
How to differentiate between cardiogenic and non cardiogenic pulmonary edema ?
Psychiatry postings :(from 27/11/2022 to 11/12/2022)
The most important thing I learnt in psychiatry postings is history taking .
Whatever be the branch we end up in there is a role of mental health to it ...
For example :
In paediatric age group we usually get to see cases like -ADHD,Mental Retardation,Temper tantrums etc.,
In women we see -disorders like pre menstrual disorders,post partum psychosis , post menopausal syndrome etc .,
In older age individuals we get to deal with :depression ,dementia etc .,
In my psychiatric postings I’ve seen some interesting cases like :
Schizophrenia
Post partum psychosis
Adjustment disorder
BPAD
ATPD
Vascular dementia
Prodrome psychosis
Depression
Alcohol dependance syndrome
Alcohol and tobacco dependance syndrome
Mixed Anxiety and Depression etc .,
To assess pts illness ..,proper history from the patient and the attendant is very crucial.
A very interesting case of visual hallucinations following a scorpion sting in a 60F :
Toxins affect various voltage-gated ion channels, principally sodium, potassium, chloride, and calcium. By acting on sodium (excitation) and potassium (blocking) channels, the toxin prolongs depolarization, mainly at the level of postsynaptic postganglionic nerve terminals of the ANS. This may cause a massive release of sympathetic (catecholamine) and parasympathetic (acetylcholine) mediators, resulting in a mixed neuroexcitatory syndrome.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8158070/
For assessing we have few scales like :
Hamilton depression scale and anxiety scales
HAM-D:
HAM-A:
MMSE:to assess the cognition of pt and how it’s improving throughout the followup and thus managing accordingly ..
-To diagnose a pt with psychiatric illness the criteria given by ICD should be met (now ICD 11 is being practiced)
-After diagnosing ...there are two options in treating the patient ...either one of them or both of them can be given ..
One is psychiatric counselling (non pharmacological strategies)
And the other is by giving medications (pharmacological)
-Few techniques like mind diversion techniques,deep breathing exercises are advised.
-Patient and support from patient’s family members is very important in controlling the psychiatric illness .
-Dealing with mental health problems is very challenging ...especially when there’s no insight ..It requires combined efforts from patients family ,health professionals and society too ...



























Comments
Post a Comment