CovidCases
Question number:1:Covid 19 with co morbidity (Pulmonology/Rheumatology)
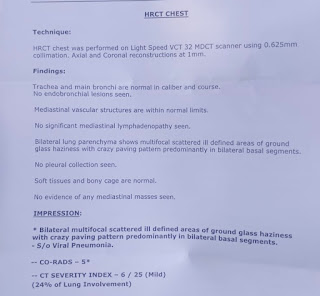
• ILD (Interstitial Lung Disease) in this patient surely is the reason for bad prognosis in this patient ,
•Since this patient is suffering from ILD for about 5 years ,and it’s association with covid pneumonia is responsible for extensive inflammatory changes in the lungs ,and I assume ILD is responsible for poor prognosis in this patient .
- Similar to SARS-CoV which caused an epidemic in 2002- 03, the novel coronavirus enters cell hosts through Angiotensin II Converting Enzyme receptor (ACE2). This receptor is found throughout the body and its pulmonary distribution explains, not only the respiratory clinical features, but also the acute respiratory distress syndrome that leads to severity of the disease.
- ACE2 receptor is found in the pancreas, both on exocrine cells and in the endocrine cells, that constitute pancreatic islets. Interestingly, its expression is also relevant in the endothelial cells of the microvasculature supplying beta-cells that produce insulin.
- As it has been postulated, upon the 2003-SARS pandemic, coronavirus spike protein enters the cells using the ACE2 receptor, initiating an inflammatory response that leads to apoptosis. Previous studies attempting to understand the pathophysiology of the SARS-CoV-2 infection over different organs and systems, have su- ggested that, following viral entrance and cell infection, ACE2 receptor is downregulated in lung tissue, which subsequently may trigger an inflammatory response.
- Although SARS-CoV-2 could directly impair insulin production of beta-cells, diminishing its function and disturb glucose metabolism, would that be enough to com- promise insulin production in a long-term manner and induce type 1 diabetes? Is there any immune mediated process? Or is ACE2 downregulation the factor at stake?
- One hypothesis could be that the cytokine storm - caused by the severe inflammatory response taking place in the lungs also targets the pancreas possibly causing diabetes .
- Other hypothesis is related to the role of the renin-angiotensin system (RAS) and its counterbalancing arm, the ACE2-Ang(1-7)-Mas axis on the development of diabetes. It has been shown previously how ACE2 decreased activity is detrimental for the development of acute respiratory distress syndrome (ARDS), verified both during the SARS-CoV epidemic as well during the current pandemic of COVID-19.
The constant touch with a medical professional is must. They should be aware of the development from mild to moderate symptoms in case any. However the underlying challenge would be associated with families having small homes to isolate themselves away from other members of the family. Elderly patients are adviced to have a oxygen cylinder handy.
Emotional challenges:
Given the mental stress of having a close family member or loved one infected with Covid, caregivers should also explore the option of therapy or counseling for themselves. Uncertainty and panic take a toll on mental health. Therapy is suggested to cope with the emotional trauma associated with coronavirus infection.
Harms of hospitalisation:
iatrogenic events such as nosocomial infections, pressure sores, delirium, functional decline, medication side effects, physical and pharmacologic restraints, and complicated care transitions. Many elderly patients are susceptible to other complications not directly related to the illness or injury for which they were hospitalized or the specific treatment of the problem.
This might be due low blood potassium as it can make you breathlessness, as it can cause the heart to beat abnormally. This means less blood is pumped from your heart to the rest of your body (even to brain).This might have lead to cerebral hypoxia and thus leading to coma
Yes, coma is related to Hypokalemia periodic paralysis as it might have caused cerebral hypoxia.
1.After cessation of sedatives, the described cases all showed a prolonged comatose state.
2.After prolonged periods of mechanical ventilation in the ICU.
The researchers have found in the study that people who recovered from coronavirus infection had a 40–60 per cent higher risk of re-admission within the next 10 days. People discharged from hospital after covid 19 appear to have increased rates of organ damage ("multiorgan dysfunction") compared with similar individuals in the general population.
Factors responsible for early recovery in covid:
•Better immune response of the patient
•Treating the symptoms as early as possible.
•No underlying comorbidities .
•Maintaining proper diet and life style habits
•Young and immunocompetent individuals have a early recovery compared to elderly.
•Decreased fever duration.( due to decreased risk of cytokine storm and further inflammatory changes )
__________________________________
Hypertension and severe obesity are common comorbidities in patients with diabetes. It is unclear whether diabetes alone contributes to increased risk of morbidity and mortality related to COVID-19. have indicated that poorer glycemic control is associated with poorer outcomes in people with diabetes
mechanisms that may increase the ability of COVID-19 to impact patients with diabetes:
higher affinity cellular binding and efficient virus entry; decreased viral clearance; diminished T-cell function; increased susceptibility to hyperinflammation and cytokine storm; and the presence of cardiovascular disease
pathogenetic link between diabetes and COVID-19. Both disease conditions involve inflammation with the release of inflammatory markers. The roles of angiotensin-converting enzyme molecule and dipeptidyl peptidase were explored to show their involvement in COVID-19 and diabetes. Pathogenetic mechanisms such as impaired immunity, microangiopathy, and glycemic variability may explain the effect of diabetes on recovery of COVID-19 patients. The effect of glucocorticoids and catecholamines, invasion of the pancreatic islet cells, drugs used in the treatment of COVID-19, and the lockdown policy may impact negatively on glycemic control of diabetic patients.
Patients with diabetes mellitus have increased predisposition to viral and bacterial infections including those affecting the respiratory tract
One of the mechanisms responsible for this predisposition is the “lazy” leukocyte syndrome, which represents impaired leukocyte function of phagocytosis (impaired immunity). This further emphasizes the likelihood of increased propensity of SARS-CoV-2 infections in diabetic cohorts
Microangiopathy in diabetes mellitus also impairs the lung compliance with consequent affectation of the gaseous exchange. This impairment may result in the proliferation of some respiratory pathogens including SARS-CoV-2
There are respiratory changes in diabetic patients that affect lung volumes and pulmonary diffusing capacity
Glycemic variability is a prognostic factor in diabetic patients with COVID-19 infection. Hyperglycemia worsens the outcome by the process of cytokine storm, endothelial dysfunction, and multiple organ injuries
In the lungs, the primary target of COVID-19, hyperglycemia leads to a rapid deterioration in spirometric functions, especially decreased forced expiratory volume in 1 second and forced vital capacity
hyperglycemic states, there is elevated glucose concentration in the respiratory epithelium which may affect its innate immune capacity. Hypoglycemia also increases cardiovascular mortality by accentuating monocytes which are pro-inflammatory and enhancing platelet aggregation
Severe hypoglycemia which may occur with strict glycemic control may worsen the overall mortality rate
suboptimal glycemic control in COVID-19 patients is correlated with higher mortality rate
Effect of COVID-19 on Diabetes:
COVID-19 infection compounds the stress of diabetes mellitus by releasing glucocorticoids and catecholamines into circulation. These worsen glycemic control and increase the formation of glycation end products in many organs and worsen prognosis
The degree of inflammatory response to COVID-19 is more marked in diabetic patients than in nondiabetic cohorts
showed that type 2 diabetic group had higher levels of inflammatory markers such as C-reactive protein and procalcitonin (57.0 and 33.3%) than the nondiabetic group (42.4 and 20.3%), respectively. Elevated C-reactive protein may serve as a marker for identifying those with high risk of death from COVID-19
D-dimer which is a marker of coagulation status was also elevated in the diabetic group compared to the nondiabetic group
The levels of these inflammatory markers have been correlated with the severity of COVID-19 infection.
To control the high range diabetes she is on insulin’s injections which have faster and effective action to control diabetes than oral hypoglycaemic drugs.
Insulin exhibits inhibitory action on ADAM-17 [35]. ADAM-17 enhances the proteolytic shedding of the enzymatic active ecto-domain of ACE2. This may suggest that insulin increases the activity of ACE2 [35] and also increases the infectivity of SARS-CoV-2
The beneficial effect of insulin may be related to its anti-inflammatory effect, which is by suppression of pro-inflammatory cytokines and increased immune mediators
Insulin use has effective glycemic control.which benefits a better prognostic results.
It is characterized by agitation, restlessness, emotional lability, and positive psychotic features such as hallucinations, illusions that often interfere with the delivery of care. It should be remembered that new-onset psychotic symptoms in older adult patients are unlikely to be a primary mental illness, and search for a pharmacological or physiological cause should be carried out.
Since this patient is a known case of htn since 2 years and had a cerebrovascular episode 2 years back
these might be have caused sleep disturbance and thus lead to icu pyschosis:
Environmental contributors include patient care, noise, light, and medications.
Patient factors, including illness severity, SOB can also play important roles
While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve.
This might be the cause for persistent hypoxia in this patient
Another possibility is that the higher risk comes not from high blood pressure itself, but from certain drugs used to treat it -- ACE inhibitors and angiotensin receptor blockers (ARBs).
The theory is based on the fact that ACE inhibitors and ARBs raise levels of an enzyme called ACE2 in your body. And to infect cells, the COVID-19 virus must attach itself to ACE2.
Coronavirus can also damage the heart directly, which can be especially risky if your heart is already weakened by the effects of high blood pressure. The virus may cause inflammation of the heart muscle called myocarditis
Hypoalbuminemia status has been associated with critically ill patients and mortality across numerous clinical settings . The pathophysiology behind hypoalbuminemia in disease state (such as pancreatitis, infection, trauma, burn, and organ dysfunction) is thought to be secondary to increased capillary permeability, decreased protein synthesis, decreased half-life of serum albumin, decreased serum albumin total mass, increased volume of distribution, and increase expression of vascular endothelial growth factor .The hallmark of severe COVID-19 includes the cytokine storm and an interplay of some of the aforementioned mechanisms
risk of getting very sick from COVID-19 is likely to be lower if your diabetes is well-managed. Having heart disease or other complications in addition to diabetes could worsen the chance of getting seriously ill from COVID-19, like other viral infections.
Viral infections can also increase inflammation, in people with diabetes. This can also be caused by elevated blood sugars, and that inflammation could contribute to more severe complications.
2.O2 supplementation with 15 L/min
3.Neb with DUOLIN+BUDDCORT 6th hourly inj.

Comments
Post a Comment