A 50 year old male with active TB
G.Sai Vidya,MBBS -IV
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 50 year old male toddy tree climber by occupation resident of yadadri has presented with chief complaints of : cough since 3 months, fever since 1 month, vomitings since 5 days,giddiness since 5days .
Patient was apparently asymptomatic 7 years back ,then on very fine day he suddenly developed episodes of vomitings and he visited to near by hospital ,after running few investigations he was diagnosed with pneumonia and assurance was given to him to stop alcohol and smoking and prescribed some medications too.He took medications for the same for one month and he stopped drinking and smoking too for that one month .Later after that one month he continued to smoke and drink again. And also got back to his daily routine .
He stopped collecting toddy from 3 years ,as his children found out that he’s drinking too much of it and they stopped him from going to work .
Cough-since 3 months ,productive cough,yellowish in color, 2-3 spoonfull in quantity (approximately),foul smelling and not bloodstained .
Cough is more during night and sputum is more in the morning.
He gets up from his sleep due to the cough.
Fever since 1month ,which is insidious in onset ,gradually progressive with no diurnal variation and relieved on taking medication.
Patient was weighing 35 kg around this time
He was diagnosed with typhoid and given medications,but the fever didn’t subside.
On 22nd March,2022:
On the night of 22nd March: The patient was unable to go to washroom on his own so asked for the help of his children,he had giddiness and became unconscious.
ORS was given and after one hour ..he had two episodes of vomiting ,which was non bilious ,non foul smelling and contained ORS .
On 23 rd March,2022:
Early in the morning ,He was taken to hospital-1 where he fell unconscious and he had involuntary micturition .
The patient’s attendants informed that his BP was low and given fluids and reffered to hospital-2 following which investigations were done and diagnosed to be having active TB.
Present complaints:cough since 3months,fever since 1month and ,giddiness since five days
On 27th pt had 4 episodes of loose motions
Past history :
not a known case of DM/HTN/Asthma/Epilepsy.
Did not receive any blood transfusions ,not underwent major surgeries .
Family history :
No history of exposure in the family
Personal history:
Diet-mixed
,appetite -decreased since 10 days
Bowel movements-regular
Bladder movements-increased frequency
Sleep-adequate
Allergies-none
Addictions-Chronic smoker since 25 years ,
Chronic alcoholic since 15 years -90 mL of whisky /day
General examination:
Pt is conscious,coherent and cooperative ,well oriented to time ,place and person
He’s poorly build and poorly nourished and weighing 40 kgs
Vitals:
Pallor:present
No icterus,cyanosis ,clubbing,generalised lymphadenopathy.
CVS:S1,S2 heard no added murmurs
CNS:higher motor functions intact
GI : scaphoid abdomen,soft non tender and no features of hepatospleenomegaly
Respiratory system:
Inspection:
Shape flattened,
Accessory respiratory muscle movements absent
Trial sign negative
Trachea appears to be central
Apex beat:appears to be near 5th intercostal space
Supraclavicular hollow present
Infraclavicular flattening present
Suprascapular wasting present
Shoulder drooping absent
No sinuses,scars or engorged veins seen
Palpation:
No Local rise of temp no tenderness
All inspectory findings are confirmed
Trachea :central,
Chest movements :reduced movements on right side
Vocal fremitus:reduced on right side
Rib crowding absent
Bony tenderness absent
Measurements:AP-6 inches ,transverse:10.5 inches
Percussion :
Right side dull note over mammary and infra nammary areas
Left side resonant
Auscultation:
Reduced breath sounds on right side
Left side normal
No wheeze ,rhonchi
Diagnosis:
Active TB
With right lower lobe pneumonia with alcoholic hepatitis with dyselectrolytemia
Hypokalemic periodic paralysis secondary to acute GE or alcohol??
Investigations:
RBS:146
HbA1c:6.5
Hb:7.58
TLC:9500
Neutrophils-90,lymphocytes-4,monocytes-3,eosinophils-3
Platelets-2.51
LFT:
Total bilirubin :2.83
Direct bilirubin:1.25
AST:230,ALT:175
A/G:1.16
ALP:230
Total proteins:4.2
Albumin:2.26
Serum electrolytes:
2D echo:
EF-55%
Trivial Tr+/no Mr , trivial Ar+
Good LV systolic function +
Diastolic dysfunction +
Usg abdomen :
Findings: 1)E/O air bronchogarm in right lung
2)E/O 5 mm hyperechoic focus noted adherent to Gb wall
Imp:
1) Gall bladder wall edema
2) right lung consolidation
3)gall bladder wall polyp
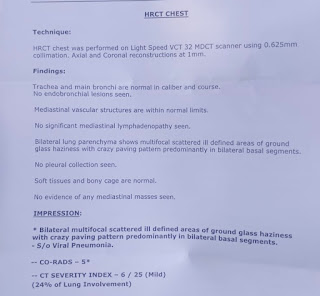
HRCT:
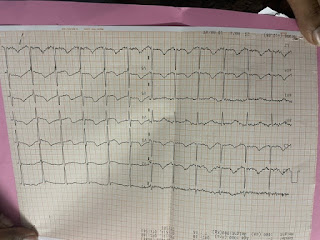
ECG:
Diagnosis:
Active TB
With right lower lobe pneumonia with alcoholic hepatitis with dyselectrolytemia
Hypokalemic periodic paralysis secondary to acute GE?alcohol?
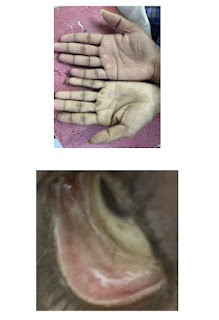
Clinical images:
Treatment:
1) Ivf ns/ rl @ 100 ml/hr
2)Inj pantop 40 mg IV/od
3)Inj zoefer 4 mg IV/sos
4)tab udilin 500mg po/BD
5)syp potlhlor 10 ml po/tid in glass of water
6)INJ monocef 1gm/IV/BD (day1)
7)2 scoop of protein powder in 100 ml milk/ water po/TID
8)Ascoryl syrup po/TID



















Comments
Post a Comment