71 year old with breathlessness
Hall ticket number:1701006050.
G.Sai Vidya
MBBS-IV
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
71 year old male ,Mason by occupation came to OPD on 1st June,2022 with chief complaints of:
Drinks toddy from 22yrs of age (1 litre / day)
Stopped smoking and toddy since 2 months.
Pt is conscious, coherent , cooperative.
well oriented to time, place and person
He is thin built and moderately nourished.
.Weight-34 kgs
.Temperature-99°F
.Pulse rate-83 bpm
.Respiratory rate-20 cpm
.BP-120/80 mm of hg
.SpO2-95%at room air
.GRBS-108mg/dl
.Pallor- absent
.Icterus-absent
.cyanosis- absent
.Clubbing- present
.Generalised Lymphadenopathy- absent
.Edema- absent
Inspection-
.Shape of chest-bilaterally symmetrical,elliptical
.Trachea- shift to right side
.Chest movements-decreased on right side
.No crowding of ribs
.No scars,sinuses,visible pulsations,engorged veins
.No supraclavicular and infraclavicular hollowing
.No intercoastal indrawing
.No kyphosis and scoliosis
Palpation-
.No local rise of temperature and tenderness
.All inspectory findings are confirmed
.Trachea-shift to right side
.Chest movements- decreased on right side
.Chest expansion-decreased on right side
.AP diameter-23cm
.Transverse diameter-30cm
.Hemithorax diameter on right side is less than that on the left side.
.vocal fremitus increased on upper part of right side
Percussion-
.Dull note heard on right upper part of chest
Auscultation-
.Normal vesicular breathsounds heard
.Decreased breath sounds on right upper lobe
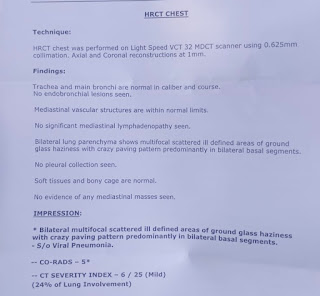
Clinical images :
PER ABDOMEN EXAMINATION :
Soft and
NO HEPATOSPLENOMEGALY
CNS :
Higher mental functions are normal
Sensory and motor examinations are normal
No signs of meningeal irritation
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD








Comments
Post a Comment