A 26 year old female with low backache and fever
Hall ticket number:1701006050.
G.Sai Vidya
MBBS-IV
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Chief complaints :
Lower back pain since 15days
Fever since 10days
History of presenting illness:
Pt was apparently asymptomatic 15days back
then she developed lower backache
Description of complaints:
Pain:
which was insidious in onset ,gradually progressive,dragging type and continuous,and it became severe later on ,pain is more during night ,pain is decreased on medication ,pain is not radiating
Fever:
She developed fever 10days back which was insidious in onset ,high grade and assosciated with chills and rigors
Vomitings:
Day 1 of admission : 1 episode of vomiting
Day 2 :6 episodes
Color-yellow,
Content-food
Not projectile
Relieved on medication
Blood in urine:
She complaints of red colored urine (blood in urine )
On the day before admission and the day one of admission
Not assosciated with pain or burning micturition
Or difficulty in passing urine
Feeling of sensation of incomplete voiding .
Facial puffiness and abdominal distension :
On day 5 of admission and subsided
Negative history:
No history of chest pain,difficulty in breathing,cough ,indigestion or heart burn .
Timeline:
Past history:
At the age of 10years she was diagnosed with Rheumatic heart disease and she underwent a surgery (CABG and mitral valve replacement)following which she took medication for 2 years and she stopped using them thereafter ,and again she’s using the medication from past 7months.
No DM,TB,HTN,Epilepsy
Personal history :
Diet:mixed
Appetite:normal
Bowel and bladder movements:regular
Sleep disturbed due to pain
No addictions
No allergies
Family history :not significant
Menstrual history :
Age of menarche:13 years
5/28 cycle ,regular,moderate flow , with clots ,no dysmenorrhea
Marital history : married for 7 years ,7months back gave birth to a girl baby
General examination:
Patient is conscious,coherent and cooperative
Well oriented to time place and person
Moderately built and nourished
Pallor -present
No icterus ,cyanosis,clubbing ,generalised lymphadenopathy,edema
Vitals:
Pulse rate:70/min
RR:20/min
BP:120/70 mmHg
Temp:afebrile
Vital chart:
Fever chart:
Fluid intake and output chart:
Systemic examination:
Per-abdomen examination
Inspection:
Shape of abdomen:normal
Movements:all quadrants are moving equally with respiration
C-section scar is present
No engorged veins ,sinuses,swellings
Striae gravidarum present
No visible gastric peristalsis
Palpation :
No local rise of temperature ,no tenderness
No palpable mass
No hepatomegaly ,spleenomegaly
Kidney not ballotable
Percussion :resonant note heard
Auscultation : bowel sounds heard
CVS :
Inspection:
Midline scar is present
Shape of chest normal
No precordial bulge
JVP not raised
No visible pulsations
Palpation: Apex beat felt at 5th ICS 2.5 cm medial to mid clavicular line
Auscultation :
S1S2 heard no murmurs
Click sound is heard without stethoscope (replaced mitral valve )
RESPIRATORY SYSTEM:
bilateral air entry - positive
Normal vesicular breath sounds heard
CNS:
Higher mental functions are normal
Sensory and motor examinations are normal
No signs of meningeal irritation
Clinical images :
Investigations:
On Day1:
Hb:9.8 %
TLC:21,900
N:83,L:7,B:2,M:8
Platelet:2.1 lakh
Normocytic normochromic anemia
LFT:
APTT :51seconds
PT:25 sec
INR:1.8
RBS:101 mg/dL
Urea:26
Sr.creatinine :1.4
Na+:141 mEq
K+:3.4
Cl_:106
On day 4
Hb:10.1
Urea :18
USG :
(Done On the day of admission)
Impression:altered echo texture and increased size of right kidney
2decho:
ECG:
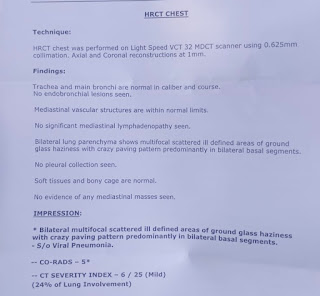
X-ray:
Diagnosis:
Acute pyelonephritis
Treatment:
IV fluid -NS,RL :75mL/hr
Inj.piptaz 2.25 gm IV TID
Inj.pan 4mg IV OD
Inj. Zofer 4mg IV SOS
Inj.neomol 1gm IV SOS (if temp >101F)
Tab.PCM 500mg /PO/QID
Tab .niftaz 100mg /PO / BD (stopped)





















Comments
Post a Comment