A 60 years old Male with SOB
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 60 year old Male came (on 18/10/22)with
c/o cough since 6 days
C/o SOB since 6 days
HOPI-
Pt was apparently asymptomatic 1 year back Then he had fever with thrombocytopenia,from then he started having SOB ,was admitted in hospital and got treated
Now after 1 year pt complaints of
Cough with sputum which is white in color ,mucoid,non foul smelling,non blood stained
Cough is more during night
C/o SOB since 3 months
SOB increases on lying down
Grade-
Palpitations +
Sweating +
A/w fever
Past history:
N/k/c/o HTN,DM,Asthma,Epilepsy ,TB
H/o surgery to spine
Personal history :
Diet mixed
Appetite normal
Bowel and bladder movements regular
Sleep disturbed (because of cough)
Smokes 9 beedis per day (since 50 years)
Smokes cigarette occasionally
Drinks toddy in summers
Drinks alcohol occasionally
General examination
Pt is c/c/c well oriented to time ,place and person
Well built and nourished
No pallor,icterus ,clubbing ,generalised lymphadenopathy
Vitals on admission -
BP-170/60mmHg
PR-50bpm
RR-32 cpm
Landolfi’s sign :
CVS-
S1S2 +
Pan systolic murmur
JVP elevated
RS -
Inspection -
Trachea appears to be central
Pattern of breathing -abdominal
Shape of chest -barrel
Palpation -
Inspectors findings confirmed
Trachea central in position
AP:Transverse =1:1.3
Bilateral air entry +
No retractions
Percussion -resonant note heard
Auscultation-wheeze +
Basal crepts+
PA :soft non tender
No organomegaly
CNS:higher motor functions intact
No focal neurological deficit
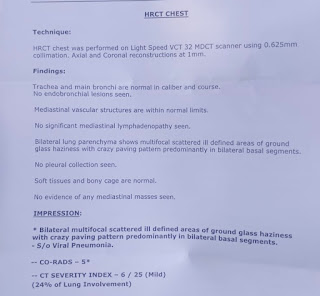
Investigations:
Serology-negative
FBS-78 mg/dL
PLBS-108 mg/dL
Blood urea -31
Serum creatinine-1.0
Na+ 145
K+ 3.8
Cl- 106
Ca :0.83
Hb-11.2 gm/dL
TLC-6,700
Neutrophils-57
Lymphocytes-33
Eosinophils -1
Monocytes-9
Basophils-0
LFT
TB-0.57
DB-0.18
AST-28
ALT-25
ALP-128
TP-5.9
Albumin -3.83
A/G-1.85
FBS-78
PLBS-108
HbA1c-6.4
Cxray-
18-10-22
20-10-22
PFT :
20/10/22
21/10/22-
2decho-
Diagnosis:
Acute exacerbation of COPD (chronic bronchitis >emphysema ) with right heart failure
GOLD-C
CAT score -7
Treatment :
(18/10/22)
Neb IPRAVENT 1 resp P/N 8th hourly
O2 supplementation (if SpO2 <92%)on RA
Tab DOLO 650 mg /PO/SOS
GRBS monitoring
BP/PR/RR/SpO2 4th hourly
(19/10/22)
S
SOB still present
Cough with sputum
No fever spikes
O
Pt is C/C/C
BP-130/80mmHg
PR-52bpm regular rate rhythm
RR-28cpm
SpO2-98on RA
CVS -S1S2 +
PSM at mitral ,aortic
S2 loud
RS -wheeze + (expiratory)
PA-soft non tender
No organomegaly
A
Acute exacerbation of COPD (chronic bronchitis >emphysema)
With RTHF
P
Nebulistation IPRAVENT 1 Respules p/n 8th hourly
O2 supplementation SPO2<92% on RA
Tab DOLO 650/PO/SOS
Tab Telma 40 /PO/OD
BP/PR/RR 4th hourly
(20/10/22)
S
SOB still present
Cough with sputum
No fever spikes
O
Pt is C/C/C
BP-100/60 mmHg
PR-48bpm regular rate rhythm
RR-26cpm
SpO2-92 on RA
CVS -S1S2 +
PSM at mitral ,aortic
S2 loud
RS -wheeze + (expiratory)
PA-soft non tender
No organomegaly
A
Acute exacerbation of COPD (chronic bronchitis >emphysema)
With RTHF > LTHF
P
Inj.DERIPHYLLIN 100 mg/IV/BD
Nebulistation IPRAVENT 2 Respules QID
Neb BUDECORT 8th hourly
O2 supplementation SPO2<92% on RA
Tab DOLO 650/PO/SOS
Tab Telma 40 /PO/OD
Tab .LASIX 40mg /PO/BD(8am—x—4pm)
SYP.ASCORYL 10mL/PO/TID
BP/PR/RR 4th hourly
(21/10/22)
Amc bed 2
S
SOB present (but reduced )
Cough with sputum
No fever spikes
Decreased sleep at night
O
Pt is C/C/C
BP-90/80 mmHg
PR-60 bpm regular rate rhythm
RR-26cpm
SpO2-97 on RA
CVS -S1S2 +
PSM
JVP raised
RS -wheeze + (expiratory)
PA-soft non tender
No organomegaly
A
Acute exacerbation of COPD (chronic bronchitis >emphysema)
P
Inj.DERIPHYLLIN 100 mg/IV/BD
Nebulistation IPRAVENT 2 Respules QID
Neb BUDECORT 8th hourly
O2 supplementation SPO2<92% on RA
Tab Telma 20 mg PO/OD
Tab .LASIX 40mg /PO/BD(8am—x—8pm)
Tab.Azithromycin 500 mg PO/OD(d1)
SYP.ASCORYL 10mL/PO/TID
BP/PR/RR 4th hourly
(22/10/22)
S
SOB present (reduced )
Cough with sputum
No fever spikes
O
Pt is C/C/C
BP-100/60 mmHg
PR-66bpm regular rate rhythm
RR-26cpm
SpO2-97 on RA
CVS -S1S2 +
JVP raised
RS -wheeze + (expiratory)
Diffuse B/L
PA-soft non tender
No organomegaly
A
Acute exacerbation of COPD (chronic bronchitis >emphysema)
P
Inj.DERIPHYLLIN 100 mg/IV/BD
Nebulistation IPRAVENT 2 Respules QID
Neb BUDECORT 8th hourly
O2 supplementation SPO2<92% on RA
Tab Telma 20 mg PO/OD
Tab .LASIX 40mg /PO/BD(8am—x—8pm)
Tab.Azithromycin 500 mg PO/OD(d2)
SYP.ASCORYL 10mL/PO/TID
BP/PR/RR 4th hourly
23/10/22
S
SOB present
Cough with sputum
No fever spikes
O
Pt is C/C/C
BP-100/60 mmHg
PR-52bpm regular rate rhythm
RR-28cpm
SpO2-97 on RA
CVS -S1S2 +
RS -wheeze + (expiratory)
PA-soft non tender
No organomegaly
A
Acute exacerbation of COPD (chronic bronchitis >emphysema)
P
Inj.DERIPHYLLIN 100 mg/IV/BD
Nebulistation IPRAVENT 2 Respules QID
Neb BUDECORT 8th hourly
O2 supplementation SPO2<92% on RA
Tab Telma 20 mg PO/OD
Tab .LASIX 40mg /PO/BD(8am—x—8pm)
Tab.Azithromycin 500 mg PO/OD(D3)
SYP.ASCORYL 10mL/PO/TID
BP/PR/RR 4th hourly
24/10/22:
S
SOB present(reduced )
Cough with sputum
No fever spikes
O
Pt is C/C/C
BP-110/60 mmHg
PR-56bpm regular rate rhythm
RR-28cpm
Temp-97.2 F
CVS -S1S2 +
GRBS-123 mg/dL
RS -wheeze + (expiratory)
PA-soft non tender
No organomegaly
A
Acute exacerbation of COPD (chronic bronchitis >emphysema)
P
Inj.DERIPHYLLIN 100 mg/IV/BD
Nebulistation IPRAVENT 2 Respules QID
Neb BUDECORT 8th hourly
O2 supplementation SPO2<92% on RA
Tab Telma 20 mg PO/OD
Tab .LASIX 40mg /PO/BD(8am—x—8pm)
Tab.Azithromycin 500 mg PO/OD(D4)
SYP.ASCORYL 10mL/PO/TID
BP/PR/RR 4th hourly
25/10/22
Advice at discharge
-Absolute smoking cessation
-Salt (<1tsp/day)and water(<1.5lit/day)restriction
-MDI spacer TIOVA 1 puff BDx2months
-Tab Deriphyllin 100mg PO/BD for 15days
-Tab Azithromycin 500 mg PO/OD for 1week
-Tab Telma 20mg PO/OD
-Tab Lasix 40mg PO/BD(8am——-4pm)
Discharge summary :











Comments
Post a Comment