A 52 year old male with background of myocardial infarction ,and pain abdomen
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 52 YEAR OLD MALE ,PRESENTED WITH CHIEF COMPLAINT OF PAIN ABDOMEN SINCE 20 YEARS
Decreased bowel movements (constipation) since 20 years
PATIENT WAS APPARENTLY ASYMPTOMATIC 20 YEARS BACK
ABOUT 20 YEARS BACK HE MET WITH AN ACCIDENT [ HE WAS HIT BY AN AUTO WHILE HE WAS GOING ON A CYCLE]
PATIENT GIVES HISTORY WHICH IS SUGGESTIVE OF LEFT HIP DISPLACEMENT/FRACTURE head of femur ?
He did not receive any TREATMENT ...which resulted in change in the gait ,prior to the trauma he used to walk normally ,the change in the gait secondary to trauma is linked below
FOLLOWING The trauma PT COMPLAINTS OF PAIN ABDOMEN
BRIEFING THE C/O PAIN ABDOMEN-
Pt complains of diffuse abdominal pain since 20 years ,insidious onset ,gradually progressive
The severity of pain has increased since 2 months which made him come to our hospital .
PT TYPICALLY GiVES H/O OF PAIN AROUND THE UMBILICUS,insidious onset gradually progressive
PAIN RADIATING TO THE BACK [BUT PAIN IN THE BACK IS OF DECREASED INTENSITY]
PAIN SUBSIDES ON TAKING MEDICATION[?]
THE INTENSITY OF PAIN NEITHER INCREASES NOR DECREASES ON TAKING FOOD
PT ALSO C/O BLOATING
BRIEFING ON REDUCED BOWEL MOVEMENTS-
PATIENT C/O REDUCED BOWEL MOVEMENTS SINCE 2 MONTHS
PASSES STOOLS ONCE IN EVERY 2-3 DAYS
FEELING OF INCOMPLETE EMPTYING OF BOWEL?
BLOOD IN STOOLS [WHENEVER He Strains to pass stools]
NOT A/W VOMITING,FEVER
NO C/O BURNING MICTURITION
Timeline of events-
PAST HISTORY-
H/O MI 6 MONTHS BACK
N/K/C/O DM,HTN,EPILEPSY, TB ,ASTHMA
PERSONAL HISTORY-
DIET-MIXED
APPETITE-NORMAL[BUT FEELING OF NLOATING DOESNT ALLOW HIM TO EAT WELL]
BOWEL MOVEMENTS -REDCUED
BLADDER MOVEMENTS -NORMAL
SLEEP-ADEQUATE
ADDICTIONS -USED TO SMOKE 1 BEEDI /DAY
STOPPED SMOKING FROM 6 MONTHS
Treatment history-
He’s on -1)Aspirin gastro resistant and atorvastatin capsules (75mg/10mg) since 6months (after the episode of MI )
2)Tab pan 40mg
FAMILY HISTORY-NOT SIGNIFICANT
DAILY ROUTINE-
WAKES UP AT 6 AM -> GETS READY FOR THE DAY->BREAKFAST[AT 10 AM][TEA,RICE WITH ANY VEG/NONVEG CURRY]->goes to work[?]->lunch at 3PM [RICE WITH ANY VEG/NON VEG CURRY]->AT 8 PM COMES BACK FROM WORK->10 PM dinner [rice with curry]-> 11 pm goes to bed
The daily routine has been same before 20 years when he was absolutely alright and it’s same even after the h/o trauma
On examination -
Pt is C/C/C well oriented to Time ,place and person
No pallor,icterus,cyanosis,clubbing,or generalised lymphadenopathy
Afebrile
BP-110/70 mmHg
PR-84 bpm
RR-16cpm
AC-77cm(at the level of umbilicus )
Rt Lt
MAC -24cm 24cm
CVS-S1S2 heard
R/S - BAE +
CNS-NFND
1. HIGHER MENTAL FUNCTIONS:
Patient sitting on the bed and responding to oral commands and questions
Speech-normal
2.CRANIAL NERVES: INTACT
3.Power
Rt UL-5/5. Lt UL-5/5
Rt LL-4/5. Lt LL-4/5
Tone -
Rt UL -N
Lt UL-N
Rt LL-N
Lt LL-N
Reflexes: Right Left.
Biceps. ++. ++
Triceps. ++ ++
Supinator. ++ ++
Knee. ++ ++
Ankle. ++ ++
4.SENSORY
crude touch N N
pain N N
Temp N N
fine touch N N
vibration N N
5.CEREBELLAR
Gait?
Coordination
Finger nose test :+
CNS examination video link
P/A
Inspection-
Shape of abdomen normal
Umbilicus -central and inverted
No visible scars,sinuses,dilated veins
Hernial orifices normal
Palpation -no local rise of temperature
Tenderness present in epigastric and umbilical region
No guarding,rigidity,rebound tenderness
No hepatomegaly,spleenomegaly
Percussion-
Resonant
Auscultation-
Bowel sounds +
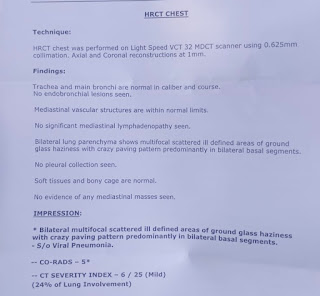
Investigations-
Hb-10.6
TLC-7,300
Neutrophils-48
Lymphocytes-37
Eosinophils-05
Monocytes-10
Basophils-00
Platelet count-1.31
CUE-
Serum creatinine -1.1 mg/dL
LFT-
Total bilirubin -0.91 mg/dL
Direct bilirubin-0.20
AST-32 IU/L
ALT-16 IU/L
Alkaline phosphate- 137 IU/L
Total proteins-6.8 gm/dL
Albumin-4.0 gm/dL
A/G ratio-1.46
Serum electrolytes and ionised calcium-
Sodium-138 mEq/L
Potassium-4.1
Chloride-103
Calcium ionised-0.97 mmol/L
Serology (anti hcv ab,HbsAg ,HIV 1/2 rapid) :negative
ECG -
2decho-
USG abdomen-
Stool sample -sent for leukocytes
(No pus cells ,no ova/cysts seen )
Upper GI endoscopy done(on 21/10/22):
Treatment-
1.Tab .Ecosprin 75 mg /PO/OD
2.Liquid Parafin 10mL/HS
3.Vital monitoring
4.Inform SOS
Discharge summary:(22/10/22)

















Comments
Post a Comment