Medicine blended assignment
I have been given the following cases to solve in an attmept to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link to the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
Question number.1: PULMONOLOGY
A)Link to patient details :
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Questions:
i)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
•Evolution of Symptomatology:
Pt had shortness of breath for past 20 years .
20 years ago - pt had her 1st episode which lasted for a week-grade II SOB-relieved on taking medication
For next 8 years she had an episode every year (around the same time i.e,January)-gradeII SOB-relieved on taking medication
12 years back -pt had a severe episode which lasted for about 20 days -grade II SOB -pt was hospitalised and SOB relieved on taking medication. (From then she’s having yearly episodes which last for about a month,which is again in January)-grade II SOB-relieved on taking medication
30 days back-her latest episode of SOB has started
( SOB is insidious in onset and gradually progressive.Initially-SOB occurred only on exertion and relieved my taking rest )
Pedal edema since 15 days
Facial puffiness since 15 days
From 2 days -she started having SOB at rest -grade IV-not relieved on medication .
From 2days- drowsiness
From 2days -decreased urine output
•Anatomical localization of problem:
Is in LUNGS(bronchi and bronchioles)
• Primary Etiology of patient’s problem :
Since she’s a farmer and she’s been having these episodes while working in paddy fields the etiological factor could be OCCUPATIONAL EXPOSURE to rice dust which is more common in Agricultural workers.
ii) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
Pharmological and non pharmacological interventions used in this patient ,their mechanism of action ,indication and efficacy over placebo are as follows:
•Head end elevation : Bed head elevation was defined as the angle of the head of the bed and was expressed in degrees of elevation above horizontal.
Mechanism of action :
Increases oxygenation ,has also been shown hemodynamic performance.
and associated with a decreased incidence of aspiration and ventilator-associated pneumonia (VAP)
Indication:
Head injury ,
Ventilator assosciated pneumonia ,
Meningitis
•oxygen inhalation:
Why is it done?
Long-term oxygen therapy is used for COPD if you have low levels of oxygen in your blood (hypoxia). It is used mostly to slow or prevent right-sided heart failure. It can help you live longer.
Oxygen may be given in a hospital if you have a rapid, sometimes sudden, increased shortness of breath (COPD exacerbation). Oxygen can also be used at home if the oxygen level in your blood is too low for long periods.
Long-term oxygen therapy should be used for at least 15 hours a day with as few interruptions as possible. Regular use can reduce the risk of death from low oxygen levels.
To get the most benefit from oxygen, you use it 24 hours a day.
Oxygen therapy has good short-term and long-term effects in people who have COPD.
Using oxygen may also improve confusion and memory problems. It may improve impaired kidney function caused by low oxygen levels.
Indications:
Chronic conditions:
A common use of supplementary oxygen is in people with chronic obstructive pulmonary disease (COPD), the occurrence of chronic bronchitis or emphysema, a common long-term effect of smoking, who may require additional oxygen to breathe either during a temporary worsening of their condition, or throughout the day and night.
Oxygen is often prescribed for people with breathlessness, in the setting of end-stage cardiac or respiratory failure, advanced cancer or neurodegenerative disease, despite having relatively normal blood oxygen levels.
Acute conditions:
Oxygen is widely used in emergency medicine, both in hospital and by emergency medical services or those giving advanced first aid.
• Intermitteny BiPAP :
BiPAP stands for bi-level positive airway pressure. It is one type of PAP, or positive airway pressure machine, that is used to maintain a consistent breathing pattern at night or during symptom flare-ups in people with COPD.
The machine pressurizes the air to a higher level than the air in the room, and so it helps a person to take in oxygen and exhale carbon dioxide. This helps them to breathe more easily, either while sleeping or when experiencing a flare-up of symptoms.
•Inj.Augumentin:
Amoxicillin/clavulanic acid is a combination penicillin-type antibiotic used to treat a wide variety of bacterial infections. It works by stopping the growth of bacteria.
binds to penicillin-binding proteins within the bacterial cell wall and inhibits bacterial cell wall synthesis.
Indications:
Amoxicillin/clavulanic acid is a combination penicillin-type antibiotic used to treat a wide variety of bacterial infections.
•Azithromycin:
Mechanism of action :
Azithromycin binds to the 23S rRNA of the bacterial 50S ribosomal subunit. It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit .This results in the control of various bacterial infections
https://www.pediatriconcall.com/drugs/azithromycin/300
Indications:
- Community-acquired Pneumonia.
- Pharyngitis or Tonsillitis.
- Uncomplicated skin/skin structure.
- Acute bacterial exacerbations of chronic obstructive pulmonary disease.
- Acute bacterial sinusitis.
- Genital Ulcer Disease (Chancroid)
- Nongonococcal or Gonococcal Urethritis and Cervicitis.
- Pelvic Inflammatory Disease
•Inj Lasix
(Furosemide)
MOA: works by blocking the absorption of sodium, chloride, and water from the filtered fluid in the kidney tubules, causing a profound increase in the output of urine
Indications:
LASIX is indicated in adults and pediatric patients for the treatment of edema associated with congestive heart failure, cirrhosis of the liver, and renal disease, including the nephrotic syndrome
•Tab .Pantop :
The mechanism of action of pantoprazole is to inhibit the final step in gastric acid production. In the gastric parietal cell of the stomach, pantoprazolecovalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion.
Indications:
- Gastro-esophageal reflux disease (GERD)
- Esophageal gastric varices bleeding prophylaxis, erosive esophagitis.
- Acid peptic disease.
- Helicobacter pylori eradication.
•Inj.Hydrocortisone:
MOA: Hydrocortisone binds to the glucocorticoid receptor leading to downstream effects such as inhibition of phospholipase A2, NF-kappa B, other inflammatory transcription factors, and the promotion of anti-inflammatory genes.
https://go.drugbank.com/drugs/DB00741
Indications:
- Collagen diseases. Systemic lupus erythematosus.
- Dermatological diseases. Severe erythema multiforme (Stevens-Johnson syndrome)
- Allergic states.
- Gastro-intestinal diseases.
- Respiratory diseases.
•Neb Ipravet:
MOA: Ipratropium acts as an antagonist of the muscarinic acetylcholine receptor.This effect produces the inhibition of the parasympathetic nervous system in the airways and hence, inhibit their function. The function of the parasympathetic system in the airway is to generate bronchial secretions and constriction and hence, the inhibition of this action can lead to bronchodilation and fewer secretions.
https://go.drugbank.com/drugs/DB00332
Indications:
Ipravent is used to relieve the symptomsof lung disease such as asthma or chronic obstructive bronchitis. It may be used in other conditions where breathing is difficult, such as after surgery or during assisted ventilation.
•Neb .Budecort:
MOA:
Budesonide is a potent topical anti-inflammatory agent. It binds and activates glucocorticoid receptors (GR) in the effector cell (e.g., bronchial) cytoplasm that allows the translocation of this budesonide-GR complex in the bronchi nucleus, which binds to both HDCA2 and CBP (HAT). This budesonide-CBP (HAT) receptor complex prevents the production of inflammatory genes (inhibition of gene transcription) that might cause bronchoconstriction. Also, the budesonide-receptor complex activates the HDCA2 increasing the gene expression, which results in the reduction of formation of the cytokines such as ILs and TNF.
It also inhibits the activation of the eosinophils by increasing apoptosis and suppresses the activation of the inflammatory cells such as mast cells, neutrophils, T-lymphocytes, macrophages, and dendritic cells. The result of the overall inhibition of ILs and TNF leads to reduced airway inflammation and hyperreactivity, causing inhibition of the bronchospasm, wheezing, and coughing.
https://www.ncbi.nlm.nih.gov/books/NBK563201/
Indications:
- Bronchial asthma.
- Bronchopulmonary dysplasia.
- Croup.
- Allergic rhinitis.
•Tab pulmoclear:
Pulmoclear Tablet is a combination of two medicines that helps the airways in your lungs stay open. It works by relaxing the muscles of these airways. This makes it easier for air to get in and out. This medicine also loosens thick mucus, making it easier to cough out.
•Inj.Thiamine :
Mechanism of Action: Thiaminecombines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
https://m.pdr.net/Mobile/Pages/drug-summary/Thiamine-thiamine-hydrochloride-2546
INDICATIONS AND USAGE:
Thiamine hydrochloride injection should be used where rapid restoration of thiamine is necessary, as in Wernicke's encephalopathy, infantile beriberi with acute collapse, cardiovascular disease due to thiaminedeficiency, or neuritis of pregnancy if vomiting is severe.
Evolution of symptomatology:
•one year ago: 2-3 episodes of seizures (mostly due to alcohol)
•4months ago: another seizure episode (most probably GTCS)
•9days back: started Sudden talking and laughing to himself
(Disability in lifting himself off the bed move around is seen.Later, short-term memory loss associated with not being able to recognize family members from time to time was observed.)
Anatomical localization :
Thalamus and hypothalamus.
Primary etiology :
Wernicke's encephalopathy is a degenerative brain disorder caused by the lack of thiamine (vitamin B1). It may result from alcohol abuse, dietary deficiencies, prolonged vomiting, eating disorders, or the effects of chemotherapy. B1 deficiency causes damage to the brain's thalamus and hypothalamus.
the deficiency of thiamine and increase in levels of toxins in the body due to renal disease is the primary etiology of the patient's problem.
I) Thiamine helps the body cells change carbohydrates into energy. It has been used
as a supplement to cope with thiamine deficiency
ii)Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system.it enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell
iii)pregabalin subtly reduces the synaptic release of several neurotransmitters, apparently by binding to alpha2-delta subunits, and possibly accounting for its actions invivo to reduce neuronal excitability and seizures.
iv)Lactulose is used in preventing and treating clinical portal-systemic encephalopathy .its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia.
v)Potchlor liquid is used to treat low levels of potassium in the body.
yes,As the patient is diabetic the chance of ulcer formation increases .in a patient of chronic alcoholic theimmune system is weak due to the affect on blood cells formation and iron absorption.due to this healing of an ulcer dampens.
__________________________________________
•7 days back- Patient had giddiness that started around 7 in the morning; subsided upon taking rest; associated with one episode of vomiting
•4 days back- Patient consumed alcohol; He developed giddiness( that was sudden onset, continuous and gradually progressive. It increased on standing and while walking.)
H/O postural instability- falls while walking
Associated with bilateral hearing loss, aural fullness, presence of tinnitus
Associated vomiting- 2-3 episodes per day, non projectile, non bilious without food particles
Present day of admission- Slurring of speech, deviation of mouth that got resolved the same day
Anatomical localization of the problem :
There is a presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology- Ataxia is the lack of muscle control or co-ordination of voluntary movements, such as walking or picking up objects. This is usually a result of damage to the cerebellum (part of the brain that controls muscle co-ordination)
Many conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain medications eg. Barbituates, stroke, tumours, cerebral palsy, brain degeneration etc.
In this case, the patient has hypertension for which he has been prescribed medication that he has not taken. Stroke due to an infarct can be caused by blockade or bleeding in the brain due to which blood supply to the brain is decreased, depriving it of essential oxygen and nutrients. This process could’ve caused the infarct formation in the cerebellar region of the brain, thus causing cerebellar ataxia.
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
B) Tab Zofer 4mg- This is ondanseteron- It is an anti emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
C) Tab Ecosprin 75mg- This is aspirin. It is an NSAID
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
D) Tab Atorvostatin 40mg- This is a statin
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
E) Clopidogrel 75mg- It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting
F) Thiamine- It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
G) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelial dysfunction in this case. High BP can also promote cerebral small vessel disease. All these factors contribute to eventually lead to stroke.
•the relation between alcohol consumption and increased risk of stroke has mainly weighed in to the formation of two types- ischaemic and haemorrhagic stroke.
Ischaemic stroke- this is more common. This Is caused by a blood clot blocking the flow of blood and preventing oxygen from reaching the brain
Haemorrhagic stroke- occurs when an aneurysm bursts or when a weakened blood vessel leaks, thus causing cerebral haemorrhage
• risk of ischaemic stroke decreases due to decreased level of fibrinogen which helps in the formation of blood clots. However, heavy alcohol intake is associated with impaired fibrinolysis, increased platelet activation and increased BP and heart rate.
•In this case, his history of alcoholism, coupled with his hypertension definitely could be a causative factor of his current condition.
_____________________________________
10 years back-Paralysis of both upper and lower limbs bilateral
1 year back-Right and left paresis due to hypokalemia
8 months backSwelling over legs
7 months back - blood infection
2 months back- neck pain
6 days back- pain along left upper limb
5 days back- chest pain, Difficulty in breathing and was able to feel her own heart beat
Anatomical localization: Cervical spine
Intervertebral discs of cervical vertebrae .
(ii)What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Reasons for recurrence of hypokalemia in this patient is :
Due to Diuretics administration
Other risk factors
Female
Heart failure
Hypertension
Low BMI
Eating disorder and alcoholism: low intake of potassium
Diarrhea, cushing syndrome
ECG changes include flattening and inversion of T waves in mild hypokalemia, followed by Q-T interval prolongation, visible U wave and mild ST depression in more severe hypokalemia.
_____________________________________
(ii)In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
_____________________________________
the reason for patient to develop ataxia in past one year is ALCOHOL
The toxic effects of alcohol are diverse. Alcohol-related cerebellar degeneration is one of the commonest causes of acquired cerebellar ataxia(ALCOHOL INDUCED TOXIC ATAXIA).
The pathophysiology remains unclear but proposed mechanisms include excitotoxicity, dietary factors, oxidative stress, compromised energy production and cell death
- Reason for IC bleed could be because of Chronic ALCOHOL CONSUMPTION resulting in ALCOHOL INDUCED Toxic ataxia .Beacuse of which patient is having Repeated falls leading to IC BLEEDING
- The impaired platelet function, together with the reduced platelet count, may contribute to the bleeding diathesis associated with chronic alcoholism and to the increased incidence and recurrence of gastrointestinal haemorrhage associated with excessive alcohol intake.
_____________________________________
(ii)What are warning signs of CVA?
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body.
- Sudden confusion, trouble speaking, or difficulty understanding speech.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
- Sudden severe headache with no known cause.
Ecospirin :
Inhibits cyclooxygenase irreversibly and prevents formation of thromboxane A2 ,Since thromboxane A2 is responsible for platelet aggregation .Using ecospirin will inhibit platelet aggregation .
Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
Rt feed RT feed is a nursing procedure to provide nutrition to those people who are either unable to obtain nutrition by mouth or are not in a state to swallow the food safely.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.
Therefore it cannot be evaluated without further details
__________________________________________
There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. . This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
_____________________________________
It could be due to Iron deficiency anemia .
Iron deficiency and iron deficiency anemia may play an important role in inducing seizures from the following mechanisms:
1. Decrease of GABA inhibitory neurotransmitter due to change in its metabolism;
2. Change in neuron metabolism;
3. Reduction of enzymes such as monoamine and aldehyde oxidases; and,
4. Impairment in oxygenation and energy metabolism of the brain
Risk factors for CVT in children and infants include:
Problems with the way their blood forms clots
Sickle cell anemia
Chronic hemolytic anemia
Beta-thalassemia major
Heart disease — either congenital (you're born with it) or acquired (you develop it)
Iron deficiency
Certain infections
Dehydration
Head injury
For newborns, a mother who had certain infections or a history of infertility
Risk factors for CVT in adults include:
Pregnancy and the first few weeks after delivery
Problems with blood clotting; for example, antiphospholipid syndrome, protein C and S deficiency, antithrombin III deficiency, lupus anticoagulant, or factor V Leiden mutation
Cancer
Collagen vascular diseases like lupus, Wegener’s granulomatosis, and Behcet syndrome
Obesity
Low blood pressure in the brain (intracranial hypotension)
Inflammatory bowel disease like Crohn’s disease or ulcerative colitis
CLEXANE (LMWH)was given to relive clot in suspission of CVST
_____________________________________
- Preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax). Reduced ejection fraction (HFrEF) – also referred to as systolic heart failure
- Heart failure with preserved ejection fraction:
 Heart failure with preserved ejection fraction (HFpEF), also referred to as diastolic heart failure, is characterized by signs and symptoms of heart failure and a left ventricular ejection fraction (LVEF) greater than 50%. Heart failure associated with intermediate reductions in LVEF (40% to 49%) is also commonly grouped into this category.
- Heart failure with reduced ejection fraction:
Heart failure with reduced ejection fraction happens when the muscle of the left ventricle is not pumping as well as normal. The ejection fraction is 40% or less. The amount of blood being pumped out of the heart is less than the body needs.
(ii)Why haven't we done pericardiocenetis in this pateint?
Pericardiocentesis is not done here Because the effusion was self healing ,It reduced from 2.4cm to 1.9 cm.
Alcohol abuse increases the risk of atrial fibrillation, heart attack and congestive heart failure
high blood pressure
Smoking
Diabetes
AV block can be associated with severe bradycardia and hemodynamic instability. It has a greater risk of progressing to third-degree (complete) heart block or asystole.
(iv)What could be the cause for hypotension in this patient?
Visceral pericardium may have thickened which is restricting the heart to expand causing hypotension
_____________________________________
• The patient was diagnosed with type 2 diabetes mellitus 30 years ago and has been taking human mixtrad insulin daily and was also diagnosed with diabetic triopathy indicating uncontrolled diabetes which is major risk factor for heart failure.
• The patient was also diagnosed with hypertension 19 yrs. ago which is also a risk factor for heart failure
• He is a chronic alcoholic since 40 years which is a risk factor towards heart failure
• The patient was diagnosed with chronic kidney disease stage IV. CKD is also one of the risk factors for heart failure
Chronic kidney disease results in decreased production of erythropoietin which in turn decreases the production of red blood cells from the bone marrow.
Patient’s with anaemia and CKD also tend to have deficiency in nutrients like iron, vitamin B12 and folic acid essential in making healthy red blood cells
The most common cause for blebs and non-healing ulcer in this patient is diabetes mellitus. CKD is also known to cause delay in healing of wounds along with poorly controlled diabetes. Anaemia can also slow down the process of healing due to low oxygen levels.
The patient is diagnosed with diabetic triopathy exhibiting sequence of neuropathy, retinopathy and nephropathy
The patient has been diagnosed with diabetic retinopathy, CKD stage IV and shows signs of diabetic neuropathy such as numbness
_____________________________________
Evolution of symptomatology:
•10 years back -underwent inguinal hernia surgery(still has on and off pain)
[pain is aggravated since 3 years]
•Since 2-3 years: facial puffiness (on and off )
•Since 1 year-Hypertension
•2 days back : SOB initially grade 2
Later progressed to grade 4 and anuria
the anatomical localization of problem is in BLOOD VESSELS;
Primary ETIOLOGY:
•Physical stress of hypertension on the arterial wall also results in the aggravation and acceleration of atherosclerosis, particularly of the coronary and cerebral vessels.
•Hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
(ii)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
•Inj.dobutamine:
Dobutamine injection is indicated when parenteral therapy is necessary for inotropic support in the short-term treatment of adults with cardiac decompensation due to depressed contractility resulting either from organic heart disease or from cardiac surgical procedures.
•Tab .Digoxin:
Digoxin is a type cardiac glycoside. It's used to control irregular heartbeats (arrhythmias) including atrial fibrillation. It can also help to manage the symptoms of heart failure, usually with other medicines.
•Inj.unfractionated heparin:
unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. As a medication it is used as an anticoagulant. Specifically it is also used in the treatment of heart attacks and unstable angina.
•Tab.Carvediol:
Carvedilol is used alone or together with other medicines to treat high blood pressure (hypertension).
•TAB. Dytor
MOA:Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
•TAB. Acitrom
MOA: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
• TAB. Cardivas
MOA:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
• INJ. HAI S/C
MOA:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
Non pharmacological interventions:
• Watch for any bleeding manifestations like Petechiae, Bleeding gums.
•APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
_____________________________________
_____________________________________
•myocardial infarction is usually due to thrombotic occlusion of a coronary vessel caused by rupture of a vulnerable plaque. Ischemia induces profound metabolic and ionic perturbations in the affected myocardium and causes rapid depression of systolic function
PHARMACOLOGICAL INTERVENTION
•TAB. ASPIRIN
MOA:Aspirin inhibits platelet function through irreversible inhibition of cyclooxygenase (COX) activity. Until recently, aspirin has been mainly used for primary and secondary prevention of arterial antithrombotic events.
•TAB ATORVAS
MOA:Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
•TAB CLOPIBB
MOA:The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
•INJ HAI
MOA:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
•ANGIOPLASTY
mechanism:Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.
Yes,because PTCA, or percutaneous transluminal coronary angioplasty, is a minimally invasive procedure that opens blocked coronary arteries to improve blood flow to the heart muscle.
__________________________________________
Torsemide is a loop diuretic
Torsemide is used to help treat fluid retention (edema) and swelling that is caused by congestive heart failure, liver disease, kidney disease
It is also helpful to treat Hyperkalemia .
(iii)Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Considering decreased urine output and history of Trans Urethral Resection of Prostate(TURP) patient is at high risk of developing UTI .
Therefore, ceftriaxone is administered prophylactically in this patient.
_____________________________________
•If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage.
•elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
The reasons for a classical 2:1 excess of serum AST activity compared to serum ALT activity in alcoholic hepatitis have been attributed to
—decreased ALT activity most likely due to B6 depletion in the livers of alcoholics
—mitochondrial damage leading to increased release of mAST in serum.
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
_____________________________________
•several factors associated with the ADHD (Attention Deficit Hyperactivity Disorder)condition, include abnormalities in the functioning of neurotransmitters, brain structure and cognitive function.
•Due to the efficacy of medications such as psychostimulants and noradrenergic tricyclics in the treatment of ADHD, neurotransmitters such as dopamine and noradrenaline have been suggested as key players in the pathophysiology of ADHD.
• Depressed dopamine activity has been associated with the condition,
Treatment strategies for ADHD:
_____________________________________
Answer:
The cause of liver abscess in this patient is mostly due to TODDY consumption .
Toddy is believed to be Independent risk factor in developing Liver abscess ,to be more specific Amoebic Liver Abscess .
(ii)How do you approach this patient ?
Answer:
Amoebic liver abscess:
Management:
•The first line treatment in uncomplicated amebic abscess should be amebicidial drugs. Metronidazole is the drug of choice and has replaced the use of emetine and chloroquine. Metronidazole is effective against both the intestinal and hepatic phase. 750 mg three times a day for 7–10 days is recommended. Abscess smaller than 5 cm in diameter respond better to metronidazole treatment.
Aspiration: Although routine aspiration is not recommended in most cases percutaneous needle aspiration is required for treatment, especially in larger abscesses.
Surgical open drainage is indicated only for those with complicated amebic abscess, e.g. secondary infection or peritonitis with perforation.
(iii)Why do we treat here ; both amoebic and pyogenic liver abcess?
Answer:
Here in this patient there was no confirmatory diagnosis to differentiate if it is amoebic or Pyogenic abscess .It most likely to be amoebic liver abscess ,but not trying not to risk if it is a Pyogenic one which when left untreated ,abscess may rupture causing severe sepsis,which is life threatening .Therefore we are treating for both the abscesses.
(iv)Is there a way to confirmthe definitive diagnosis in this patient?
•Cysts of E.histolytica in stools of patients ( in only 15% of hepatic amoebiasis )
•SEROLOGICAL : positive haemagglutination test is quite sensitive and useful for diagnosis of amoebic liver abscess
The diagnosis of amebic liver abscess was based on four or more of the following criteria:
(i) a space-occupying lesion in the liver diagnosed by ultrasonography and suggestive of abscess,
(ii) clinical symptoms (fever, pain in the right hypochondrium (often referred to the epigastrium), lower chest, back, or tip of the right shoulder),
(iii) enlarged and/or tender liver, usually without jaundice,
(iv) raised right dome of the diaphragm on chest radiograph, and
(v) improvement after treatment with antiamebic drugs (e.g., metronidazole).
i)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
Evolution of symptomatology:
Pt was asymptomatic 3 years back
3 years ago-he was diagnosed with hypertension
21 days back- he received vaccination at local PHC Following which he had fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
18 days ago- complained of similar events and went to the local hospital, it was not subsided upon taking medication(antipyretics)
11 days ago - patient complains of Generalized weakness ,facial puffiness and periorbital oedema. Patient was in a drowsy state
4 days ago-
• patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
• the same evening patient’s periorbital oedema progressed
• serous discharge from the left eye that was blood tinged
•oral and nasal foul smelling was present
•was diagnosed with diabetes mellitus associated with DKA (diabetic keto acidosis)
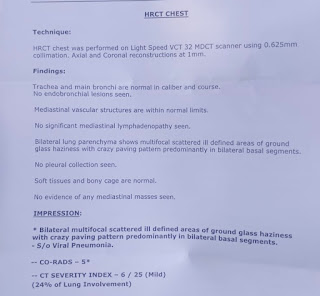
• On CT :
Preseptal cellulitis is observed
Acute infarcts in frontal and temporal lobes seen
Soft tissue swelling in maxillary sinus and mucosal thickenings of sinus seen
Following Ent referral and KOH mount:
The patient was diagnosed with acute oro rhino orbital mucormycosis
patient was referred to a government general hospital
patient died 2 days later
Anatomical localisation of the problem :
Is the sinuses and the brain
• Acute infarcts in frontal and temporal lobes
•Soft tissue swelling in maxillary sinus and mucosal thickenings of sinus
Primary etiology of patient’s problem :
•The factors that are responsible are :
Mucormycosis and
Uncontrolled diabetes associated with diabetic ketoacidosis
Diabetes mellitus tends to change the normal immunological response of body to any infection in several ways. Hyperglycemia stimulates fungal proliferation and also causes decrease in chemotaxis and phagocytic efficiency which permits the otherwise innocuous organisms to thrive in acid-rich environment. In the diabetic ketoacidosis patient, there is an increased risk of mucormycosis caused by Rhizopus oryzae as these organisms produce the enzyme ketoreductase, which allows them to utilize the patient's ketone bodies.It has been established that diabetic ketoacidosis temporarily disrupts the ability of transferrin to bind iron, and this alteration eliminates a significant host defense mechanism and permits the growth of Rhizopus oryzae
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5754995/)
Why did this condition appear all of a sudden ? Why did he develop this condition following vaccine ? Is it the post covid vaccine complication in uncontrolled hyperglycaemia associated with DKA?
It could be due to undiagnosed diabetes associated with DKA ,DKA left untreated might have lead to this condition .
(ii)What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer:
• Inj. Liposomal amphotericin B according to creatinine clearence :
MOA: binds to ergosterol in the fungal cell membrane, which leads to the formation of pores, ion leakage and ultimately fungal cell death.
• itraconazole adjusted to his creatinine clearance:
MOA: Itraconazole acts by inhibiting the fungal cytochrome P-450 dependent enzyme lanosterol 14-α-demethylase. When this enzyme is inhibited it blocks the conversion of lanosterol to ergosterol, which disrupts fungal cell membrane synthesis.
approach to treat this case :
Management of Mucormycosis:
- Intravenous Amphotericin B is the drug of choice for initial therapy
- Posaconazole or Isavuconazole is tased as stepdown therapy for patients who have responded to Amphotericin B
- Posaconazole or Isavuconazole can also be used as salvage therapy for patients who don’t respond to or cannot tolerate Amphotericin B
- Surgery- Aggressive surgical debridement of involved tissues should be considered as soon as the diagnosis of any form of Mucormycosis is suspected.
- Diabetic ketoacidosis requires insulin and volume repletion with intravenous fluids.
Management of DKA:
Fluid replacement
At the hospital, your physician will likely give you fluids. If possible, they can give them orally, but you may have to receive fluids through an IV. Fluid replacement helps treat dehydration,which can cause even higher blood sugar levels.
Insulin therapy
Insulin will likely be administered to you intravenously until your blood sugar level falls below 240 mg/dL. When your blood sugar level is within an acceptable range, your doctor will work with you to help you avoid DKA in the future.
Electrolyte replacement
When your insulin levels are too low, your body’s electrolytes can also become abnormally low. Electrolytes are electrically charged minerals that help your body, including the heart and nerves, function properly. Electrolyte replacement is also commonly done through an IV.
(iii)What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Answer:
Mucormycosis is opportunistic infection that occurs in diabetics,immunocompromised individuals etc,.
We know that India has high incidence of Diabetes .
The reason for the increasing incidence in India is being mainly attributed to a continued increase in the patient population with uncontrolled diabetes.
https://www.researchgate.net/publication/263187827_Epidemiology_of_Mucormycosis_in_India
•it is also due to overuse of steroids in management of covid pneumonia is also the reason .
Steroids being immunosuppressants and favouring the growth of fungus leading to mucormycosis.

Comments
Post a Comment